As many as one-in-ten children in Gavi-supported countries do not receive a single-dose of routine vaccines. To reach these missing millions in the 5.0 Strategy, Gavi will bring a much stronger focus on reaching the most marginalised by strengthening primary healthcare systems, building and sustaining community demand, addressing gender barriers and using innovation to ensure that immunisation services reach these children. The goal: to reduce the number of zero-dose children by 25% by 2025, and by 50% by 2030.
Zero-dose community
A platform for experts striving to reach zero-dose children with life-saving immunisation.
- Introduction
-
Gavi’s 5.0 vision of leaving no one behind with immunisation by 2030 is inspired by the Sustainable Development Goals (SDGs) and aligned to Immunisation Agenda 2030 (IA2030). Equity is the organising principle of the Gavi 2021-25 (Gavi 5.0) strategy and underpins the broader “leave no one behind” ambition of the global development agenda.[1] The Immunisation Agenda (IA 2030) places priority and focus on reaching the most marginalised and vulnerable populations to ensure that all children receive all vaccines.
Routine immunisation programmes, especially in low- and middle-income countries, strengthen access to and delivery of primary health care (PHC) as a pathway towards achieving Universal Health Coverage (UHC). Immunisation also contributes to global health security and achieving 14 of 17 SDGs.
Gavi 5.0 Strategy: “Leaving no-one behind with immunization” by reaching zero-dose and missed communities
The equity goal: Health systems sustainably reach all zero-dose and under-immunised children and their communities with the full range of vaccines as the first step towards providing integrated Primary Health Care (PHC) services.
- High quality immunisation services are sustainably available to missed communities where and when they are needed
- All vaccines in the national schedule along the life course are available to missed communities
- Caregivers bring children to vaccination services
- Continuous improvements of programmes in range and quality of services
These commitments follow decades of progress made by governments with support from the global health community and build on the achievements of the Alliance’s “Coverage & Equity” agenda in Gavi 4.0. In 2000, just 47% of children in lower-income countries received basic (DTP3) vaccines. In Gavi-eligible countries, coverage of key vaccines increased by 3 percentage points from 2015 to 2019, and the number of zero dose children reduced by 14% (Figure 1). In 2019, coverage for the same countries reached 82% before sliding back to 78% due to the COVID-19 pandemic.[2],[3]
Immunisation now reaches more communities than most other routine health interventions though we are still far from the goal of leaving no one behind with immunisation. Communities not receiving immunisation services are likely not receiving any other essential health services.[4] In 2020, approximately 16 million of the 72.9 million children targeted with Gavi support did not receive their third dose of DTP-containing vaccine. 78% of these children, 12.4 million in total, did not receive a single dose of DTP-containing vaccines and are defined as “zero-dose.”[5] Pre-pandemic analyses suggest nearly 50% of vaccine preventable deaths occur among zero-dose children.[6] Two-thirds of these children live in extremely poor households suffering from multiple deprivations including lack of access to reproductive health services, water and sanitation.[7]
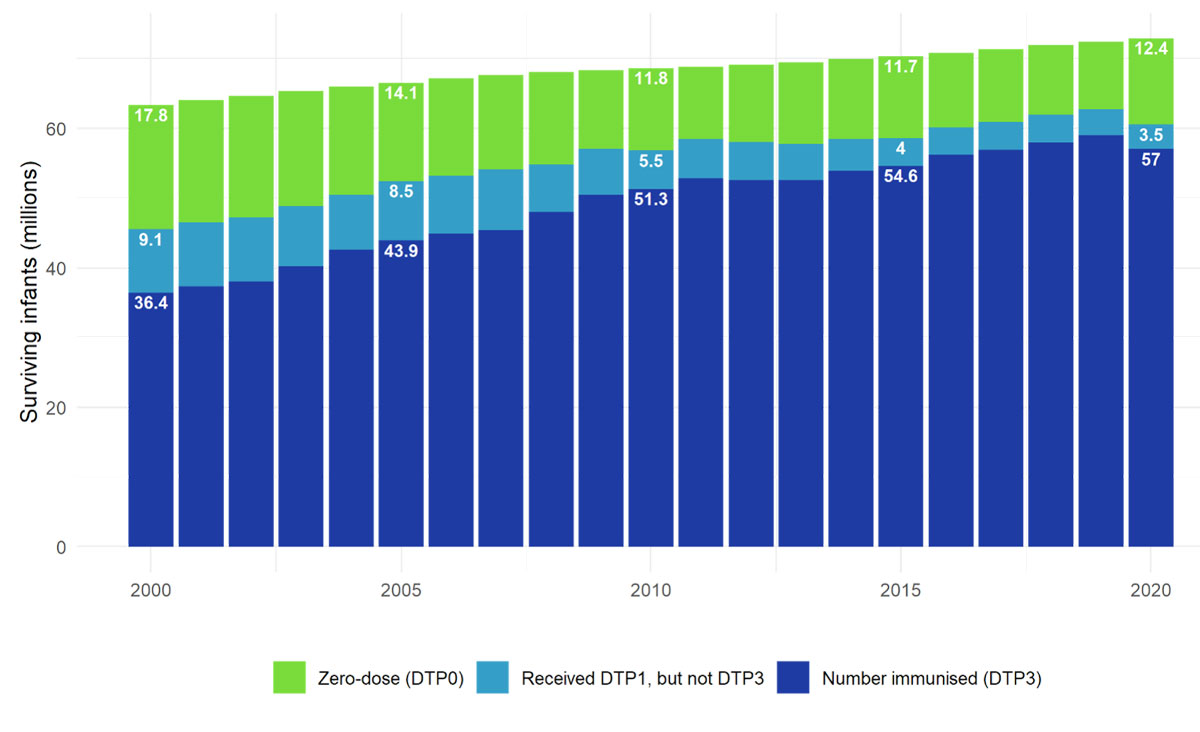
Figure 1: Progress in reaching zero-dose and under-immunised children in Gavi implementing countries (Gavi57 country data).
The most vulnerable populations have been hardest hit by the pandemic. Therefore, Gavi’s mission to save lives by strengthening routine immunisation services and reaching zero dose children and missed communities has become even more urgent, along with supporting countries to deliver COVID-19 vaccines.
COVID-19 related disruptions led to a 4 percentage point drop in coverage in 2020. The estimated decline in DTP3 coverage was almost entirely due to a nearly 30% increase in zero-dose children, highlighting the importance of reaching children with a first dose of vaccine. After a successful reduction of 1.7 million zero-dose children over the previous four years, 2020 saw an increase of 3.1 million zero-dose children and 3.0 million underimmunised children in Gavi68 countries compared to 2019.
Available data suggests the largest disruptions were concentrated in Q2 2020, with the majority of countries restoring routine immunisation services in the second half of the year. Over three-quarters of under-immunised children are now zero dose, heightening the risk of child deaths, disease outbreaks and medical impoverishment.
Improvements in routine immunisation coverage has contributed to a large reduction in child deaths and recent analysis of immunization coverage trends show the importance of centering approaches on equity and underserved communities in order to avoid a further plateau of coverage in the coming decade.[8] It can also be the first step towards comprehensive primary healthcare – providing opportunities for multi-agency and cross-sector coalitions to drive broader social change including gender equality. This ambition reflects the central shift in the Gavi 5.0 strategy of reaching zero-dose children and missed communities with a full course of vaccines in conjunction with stronger PHC services and an increased focus on programmatic sustainability.
Once children receive one dose of a vaccine, most children go on to receive more vaccines. A recent study found that over two-thirds of children reached with at least one dose of a vaccine went on to become fully vaccinated with all four basic vaccines (BCG, Polio, DTP and MCV).[9]
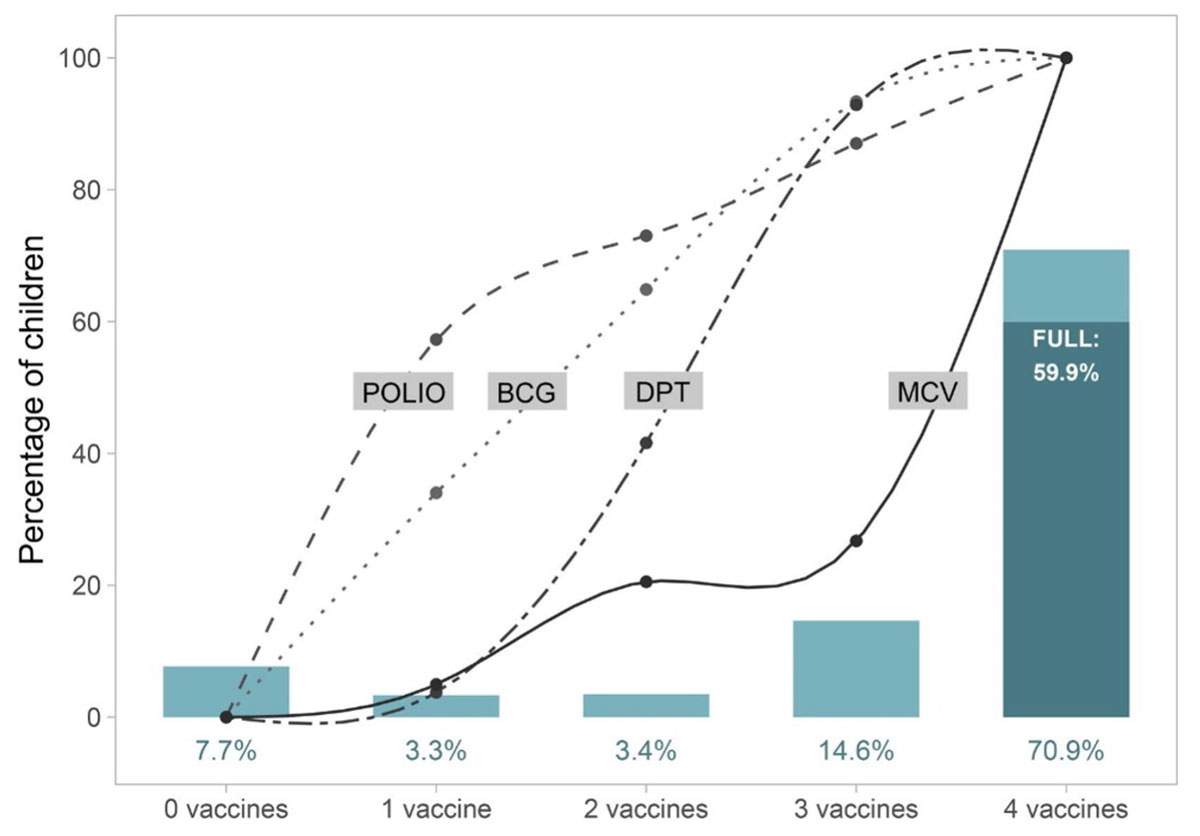
Figure 2: Two-thirds of children reached with at least one dose of a vaccine go on to become fully vaccinated
The importance of immunisation reaching all children is paramount and ensures all children to have an equal chance of being healthy and productive members of society. Vaccination, because of its preventative nature, averts illness and provides particularly significant benefits to zero-dose communities which may lack access to affordable, quality curative care while being at higher risk of vaccine-preventable diseases. Immunised children are also more likely to grow up healthy and to enjoy their right to survival and development. Vaccinated children have higher cognitive abilities, miss school less and are in school for longer, and have better nutrition and education outcomes – all of which translates into better earning potential and productivity as an adult.[10]
- Who are zero-dose children and missed communities?
-
Missed communities are often deprived of other basic services and face other socio-economic and gender disparities.[11] The lack of access to immunisation is closely linked to extreme poverty: nearly two-thirds of zero-dose children in Gavi-supported countries live in households surviving on less than US$ 1.90 per day – the international poverty line.[12] Zero-dose children live in communities that suffer not just from high child mortality but also high maternal deaths. Mothers of children who miss out on basic vaccines are 47% less likely to receive antenatal care or skilled birth attendance.[13] The Global Action Plan for Health Lives and Wellbeing for All - Progress Report recognizes zero-dose child as a marker of communities facing multiple deprivations.[14]
With low immunisation coverage, these communities are vulnerable to recurrent vaccine-preventable disease outbreaks, such as measles, which can spread rapidly, worsening health and development outcomes. One in eight children in Gavi-supported countries are zero-dose, yet these children account for nearly half of all children dying from vaccine preventable diseases.[15] Communities with zero-dose children also have a significant number of under-immunised children: data shows a high degree of overlap between subnational areas with high numbers of zero-dose and high numbers of under-immunised children.[16]
The underlying causes for a child to be zero-dose are wide-ranging and include socio-economic factors, deeply entrenched barriers and vulnerabilities related to poverty, conflict, forced migration, homelessness and religious or cultural marginalisation. There may be systemic gaps in delivering reliable primary healthcare services or in addressing vaccine hesitancy. Gender barriers to immunisation continue to be varied including mothers’ access to education, household decision-making for healthcare, gender-based violence, child marriages and teenage pregnancies. Gavi’s Gender Policy aims to address these barriers through research, investment, and partnerships.
Communities that face these barriers exist in many geographic settings. Approximately 45% of the 9.7 million zero-dose children live in urban/peri-urban, remote rural or conflict settings, while the remaining are in non-specific settings.[17] The contextual challenges of these settings have been studied by the wider immunisation community, including by the Equity Reference Group.
Geographic contexts with high concentrations of zero-dose children
Informal and peri-urban settlements are characterised by high population density, high mobility and an uneven distribution of wealth and services. There is a high risk of disease transmission and outbreaks in large, growing, densely populated areas with mobile and transient populations.
Residents of remote-rural areas face barriers including service access, weaker infrastructure, economic deprivation and limited access to high quality health services.
Approximately 1/5 of zero-dose children in Gavi-supported countries live in conflict settings/ areas. Conflict destabilises countries, disrupting essential infrastructure and resources needed to provide care and access to services.
Source: WorldPop analysis of IHME subnational immunization coverage estimates
This means that successfully reaching zero-dose and under-immunised communities will require highly differentiated, targeted sub-national strategies and a strong learning agenda. Learnings from Gavi’s 4.0 agenda show a varied but often increased cost in reaching these communities with tailored services. As part of realising the vision of Gavi 5.0, Gavi will advocate to identify and reach zero-dose and under immunized children, and provide targeted funding and technical assistance to accelerate further progress.
- Investing to reach the zero-dose and missed communities
-
Reaching zero-dose and under-immunised children means reaching the missed communities they are part of and building the link to the healthcare system and essential services. Significant investments must be made to reach children with immunisation across complex, low-coverage and difficult settings and build a recurring touchpoint with the health system. The investments in Gavi-supported countries aim to make progress towards the Immunisation Agenda 2030 goal of reducing the number of zero-dose children by 50% by 2030.
Since 2001, Gavi has provided a breadth of support to eligible countries, including support for health systems strengthening, vaccine introduction grants, technical assistance, operational costs in campaigns, cold chain support and private sector partnerships and innovations. All these streams of support offer a lever to achieve the vision of leaving no one behind and are in support of countries’ National Immunisation Plans and health sector strategies (Refer to Annex B).
In addition to traditional support, the Equity Accelerator Fund (EAF) - a new dedicated fund for accelerating the 5.0 equity agenda and investments in zero-dose communities - is now available for interventions aimed at reaching the most at-risk communities.
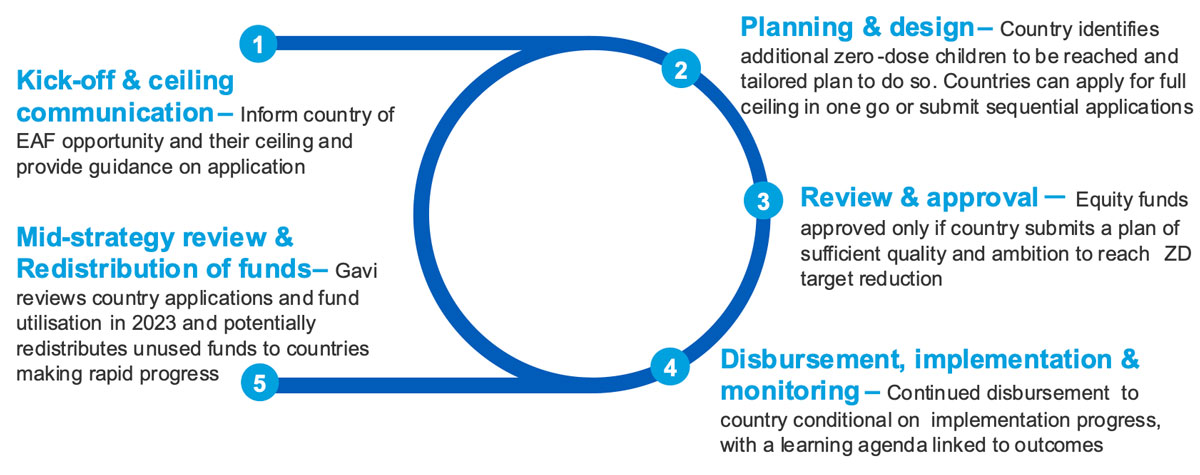
Figure 3: Overview of EAF Funding Mechanism
Part of the EAF will be allocated to a new multi-country initiative to reach zero-dose children and missed communities in fragile, conflict and cross-border settings outside government reach, with a new partnership approach. The geographic focus of this support will be to the Sahel region and Horn of Africa due to the high number of zero-dose children residing in these regions because of prolonged humanitarian crisis, conflict, and displacement.
- Delivering immunisation to zero-dose and missed communities
-
A critical element in the execution of the new approaches and the delivery of the strategy is its design, consisting of holistic and context-appropriate interventions under the leadership of eligible countries and informed by engagement of civil society and communities. A simple 5 step framework will serve as the basis for Gavi investments:
“Identify – Reach – Monitor – Measure - Advocate”
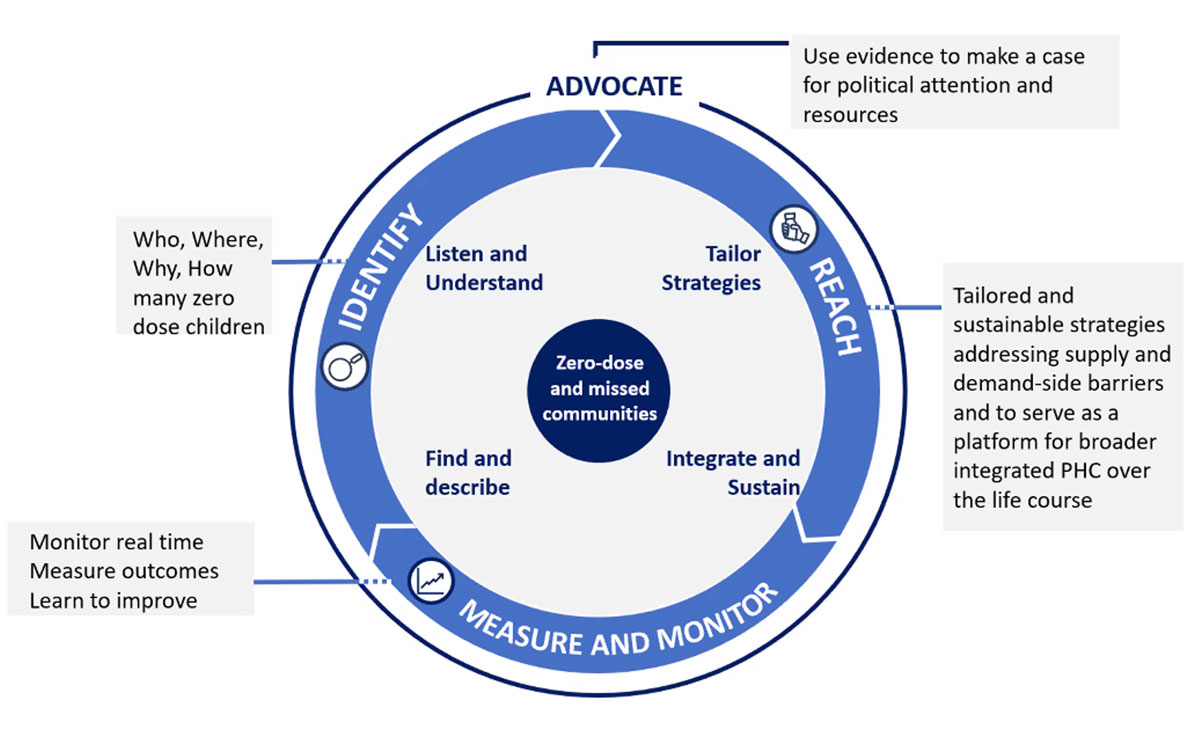
Figure 4: Using a Zero-Dose Strategy to Strengthen Primary Health Care across the Life Course
This framework provides guidance on key questions to identify challenges at the country level, potential interventions to be supported by the Gavi Alliance and a set of useful tools to guide the development of a strategy to reach zero-dose children and missed communities. The IRMMA framework draws from a wealth of existing evidence and guidance from the World Health Organization, UNICEF and others.
- Identify (Listen and Understand; Find and Describe): A clear understanding of which, where, why, and how many zero-dose children and missed communities have not been reached, demonstrating data sources used to identify the populations. Interventions including triangulation of existing subnational data, both within immunisation and other sectors (including nutrition and education), better enumeration of the distribution of zero-dose children, and geospatial mapping can help countries to identify these children and the barriers that prevent them from receiving Immunisation.
- Reach (Tailor strategies; Integrate and Sustain): Developing a coherent strategy that addresses the main barriers to service availability and service utilisation. It will be imperative that country COVID-19 response and recovery plans prioritise essential health services such as immunisation with a particular focus on missed communities with zero-dose and under-immunised children.
- On service availability (supply side barriers): tailored, quality and sustainable service delivery strategies should be designed for missed communities, grounded in strong routine immunisation and utilising the full spectrum of approaches, from fixed-post immunisation to outreach, mobile strategies, periodic intensification of routine immunisation, child health days and other supplementary activities. This should be integrated within the Primary Health Care approach.
- On service utilisation (demand side barriers): innovative and tailored strategies should be developed and scaled up to engage communities, harness behavioural insights and improve the service experience of caregivers to ensure services meet their needs. This will be even more important in countries where COVID-19 has increased vaccine concerns and generated new rumours and mistrust of immunisation, pushing up the number of zero-dose children. Countries should pay particular attention to addressing gender-related barriers which hinder access to immunisation or prevent mothers, who are often the primary caregivers, from bringing their children for vaccination (e.g. due to unsuitable timing or inconvenient location of immunisation services, experience of poor service, stigmatisation).
- Monitor/Measure and Learn: Programmes should regularly track and review progress in a timely manner to facilitate learning and course correction from programme implementation. This includes improving measurement, such as strengthening more rapid feedback and community monitoring, inclusion of operational data into health information systems and better use of this data from country to community level, periodically supplementing these routine data with targeted sub-national surveys, implementation research and assessments. For example, this could include scaling up dashboards for district-level immunisation monitoring, strengthening data triangulation, and introducing real-time campaign monitoring to identify underimmunised children. Using these data to generate insights and inform regular monitoring and review discussions from country to community levels.
- Advocate: Strong political leadership is one of the most important factors in catalysing rapid progress on immunisation equity. Governments should mobilise and prioritise primary healthcare resources towards zero-dose children and missed communities, utilising immunisation as a pathfinder for building universal primary healthcare. The advocacy approach will include wider and more sustained engagement on missed communities with government actors, partners, and new context-specific partnerships.
A full database of resources and guidance connected to the IRMMA framework is available at this link.
Partnerships
Building a global movement for equity and reaching zero-dose and missed communities will require a strong engagement with country governments, local authorities, the Alliance partners, civil society, advocacy platforms and actors outside of immunisation. The focus on advancing equity will be a priority of our dialogue and leadership engagements with country stakeholders to promote a tailored and informed approach for zero-dose children within country systems and communities.
Gavi has developed a new strategy to strengthen engagement with Civil Society Organisations. The partnerships expand an already robust platform of collaboration across the Alliance to reach children in missed communities. This approach is informed by evidence which shows interventions delivered at the community level are delivered more equitably.[18] Policy and advocacy work is already underway to socialise, position and amplify the zero-dose and missed communities focus in strategic global and regional policy areas.
The expansion of partnerships is particularly critical in humanitarian and fragile settings where working through national governments may not always respond to the needs of communities. To complement the expertise of existing partners and to support the Gavi 5.0 strategy and ambition, new operating agreements have been signed with humanitarian organisations, including International Organization for Migration, UNOPS, the International Rescue Committee, Save the Children, UNHCR and the International Federation for the Red Cross/Crescent. A deliberate focus is placed on building local capacity to sustain services in these contexts.
Innovative approaches and technology
Technological and operational innovation are opportunities to improve access to and utilisation of services by missed communities including: the use of Geographic Information System (GIS) satellite imagery and digital maps to estimate populations and develop microplans, the use of smart phones to send SMS messages as reminders to caregivers and for tracking defaulters, as well as modifying days and times of services to accommodate caregivers.[19] Gavi will leverage its private sector partnerships to effectively source and adapt solutions that can support priorities at scale and support the creation of an enabling environment for innovation.
Furthermore, innovative products, services and practices are critical to reach zero-dose children and missed communities. The Alliance has prioritized three key product innovations as part of the Vaccine Innovation Prioritisation Strategy (VIPS).
Continuous learning
Effective prioritisation and reach of zero-dose and under-immunised communities will be contingent on learning. The shifts in how the Alliance approaches learning is reflected in the Gavi 5.0 Learning System, which includes a four-step process:
- Anchored in the Gavi 5.0 Theory of Change, Learning Priorities (LPs) established through a consultative process form a focused set of questions for which evidence will be generated. At the country level, LPs will be reflected in the Monitoring and Learning (M&L) Plan.
- Targeted generation of evidence to address the LPs through deployment of a coordinated set of tools (e.g., monitoring, evaluation, targeted assessments, and other forms of learning) tailored to meet the needs of the data users in terms of timeliness and type of evidence as well as providing efficiency in the use of available resources to support learning.
- Practicing more holistic data triangulation and synthesis to bring together the evidence generated through different tools, systematically translating these data across sources to yield new and more comprehensive insights made accessible to users at the right time to enable learning.
- Emphasising timely and more rigorous use of evidence to maximise the continuous improvement of performance at both Alliance and country levels. Improving the packaging of insights and products tailored to meet the needs of different users, more engagement and opportunities to share key learning as it emerges and when it is needed providing the ‘right information, right time, right people’. This includes strengthening mechanisms for stock taking at key points to assess progress and performance with feedback loops and aligned with the Gavi support and governance cycles.
As countries design holistic and context-appropriate interventions and implement their approaches to achieve equitable delivery, the Alliance and partners are committed to provide expertise and investment to match their ambition and ensure all children receive all vaccines.
Defining the zero-dose child
Zero-dose children are those that have not received any routine vaccine. For operational purposes, Gavi defines zero-dose children as those who lack the first dose of diphtheria-tetanus-pertussis containing vaccine (DTP1).
An under-immunised child is defined as those missing the third dose of diphtheria, tetanus and pertussis (DTP)-containing vaccine (DTP3).
Missed communities are home to clusters of zero-dose and under-immunised children. These communities often face multiple deprivations and vulnerabilities, including lack of services, socio-economic inequities and often gender related barriers.
A call to action
Of the 16 million infants that were not fully vaccinated with DTP3 in 2020, 12.4 million did not receive an initial dose, pointing to a lack of access to immunisation services.
A further 3.5 million were partially vaccinated without completing the required 3-dose schedule in the first year of life.
ANNEXES
- A: Gavi 5.0 Strategy
- B: The different types of Gavi support and their role in improving the equity of immunisation and reaching ZD children
Sources
[1] SDGs Report 2020
[2] WHO and UNICEF estimates of national immunization coverage (WUENIC), 2021
[3] Gavi Eligibility
[4] Tracking Universal Health Coverage: 2017 Global Monitoring Report
[5] WHO UNICEF Immunization Coverage Estimates 2019 revision for 57 countries supported by Gavi in 2021-25
[6] Prevent, Protect, Prosper - Gavi Alliance 2021-25 Investment Opportunity
[7] International Center for Equity in Health analysis of DHS/MICS survey data
[8] Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: a systematic analysis for the Global Burden of Disease Study 2020, Release 1
GBD 2020, Release 1, Vaccine Coverage Collaborators Open Access. Published:July 14, 2021DOI:https://doi.org/10.1016/S0140-6736(21)00984-3
[9] Zero-dose children and the immunisation cascade: Understanding immunisation pathways in low and middle-income countries, 2021
[10] IVAC, Vaccinating Children: Helping children think, learn and thrive
[11] World Bank, Global Economic Prospects, January 2021
[12] Prevent, Protect, Prosper- Gavi Alliance 2021-25 Investment Opportunity
[13] International Center for Equity in Health analysis of DHS/MICS survey data
[14] SDG3 GAP 2nd Progress Report
[15] Gavi Secretariat analysis of WHO estimates of child causes of death, co-coverage of vaccines as estimated from DHS/MICS, and WUENIC coverage estimates
[16] Analysis of Institute for Health Metrics and Evaluation (IHME) district-level coverage estimates shows that for every 1pp increase in % zero-dose, there is a 0.6 pp increase in DTP drop-out rate on average in Gavi-supported countries
[17] WorldPop analysis of IHME subnational immunization coverage estimates
[18] Leventhal, Daniel G. et al “Delivery channels and socioeconomic inequalities in coverage of reproductive, maternal, newborn, and child health” Lancet Global Health. Published online May 26, 2021 https://doi.org/10.1016/S2214-109X(21)00204-7